Anal warts are caused by infection of the anus by the Human Papilloma Virus (HPV), the most common sexually transmitted disease. Warts affect the area around and inside the anus, but can also develop on the skin of the genital area and on the perineum. They first appear as tiny spots, often as small as a pinhead. They can grow quite large and cover the entire anal area.
It is worth noting that when warts are present on the skin around the anus there is a high chance of warts coexisting inside the anus as well. For this reason, in order to fully treat the problem, a man who has warts around the perioral and inner area of the anus should be screened with a high-resolution rectoscopy. The warts extend to a distance of 5-7cm from the anus and no deeper as it has been clarified by scientific studies that the HPV virus infects the cells of the anus, but not the cells of the intestine.
In addition to anal warts, the HPV virus (in some people) causes precancerous lesions in the anus called malformations. If these are not treated in time there is a 10-15% chance that they will develop into anal cancer within 3-5 years. Most warts can be easily diagnosed with a simple rectoscopy. But anal malformations are almost impossible to detect in the same way. This is because these lesions are flat and their colour is similar to that of normal anal mucosa.
For this reason, patients who have warts in the anus must undergo a high-resolution anoscopy using acetic acid, a special liquid that colours the malformations and allows them to be identified under the microscope. Consequently, colonoscopy, rectoscopy and simple rectoscopy have no place in the identification of lesions caused by HPV (warts and particularly anal malformations).
It is of no importance to cauterize only the perianal warts as one should always look for the intraprostatic warts as well as the anal malformations with High Definition Proctoscopy because otherwise the intraprostatic lesions that are not treated constitute a reservoir of HPV, which constantly transmits viral load outwards causing frequent recurrences. In addition, when there are warts on the anus, it is important to check for warts on the penis, vulva and oropharynx.
The HPV virus
HPV (Human Papilloma Virus) infection is the most common sexually transmitted infection in the modern world and affects both men and women. There are about 150 types of HPV that affect different parts of the body. About 30 types of HPV (genital types) can affect the anus, genitals, mouth, throat, penis, scrotum, perineum, vulva, vagina and cervix.
These types are divided into 2 categories. The first category includes low risk viruses that cause warts and low grade intraepithelial lesions that are now considered not to develop into malignancy. The second category includes the high risk types, which cause the high-grade intra-epithelial lesions or malformations of the anus, which are considered precancerous as they may develop into anal cancer.
It is thought that around 80% of the sexually active population is at risk of contracting this infection at some point in their lives. About 15 types are considered “high risk” and in particular two types (16 & 18) are most commonly found in cases of anal malformations or cancer.
HPV is transmitted from person to person, usually through sexual contact. In particular, HPV can be transmitted by having vaginal, anal or oral sex with someone who carries the virus. It is most often transmitted during vaginal or anal sex. It is also spread through close skin-to-skin contact during sex by simple skin or mucous membrane contact, by contact with fluids of an infected person or even by objects on which the virus is found (e.g. sex aids). A person with HPV can pass the infection on to someone even when they have no signs or symptoms. For these reasons, condom use is essential, but it does not offer complete protection against HPV infection. Finally, the virus can be transmitted to the same person from one area to another (e.g. from the genitals to the anus and vice versa) by rubbing, scratching or even wiping after defecation.
Who is at risk of developing anal warts?
Anal warts, like HPV infection, are very common in both men and women. Men and women are more likely to develop anal warts if they:
- Do not use a condom during sexual intercourse
- Have multiple sexual partners
- Have anal intercourse
- Have or have had sexual intercourse with a person infected with the virus
- Started having sexual intercourse at an early age
- Do not have a strong immune system (HIV-positive, transplant patients, patients on chronic immunosuppressants or cortisone for various diseases, etc.)
- Smoke
- Also all women with malformations or cancer of the lower genital tract (cervix, vagina or vulva) have an increased chance of developing HPV lesions in the anus as well. Finally, warts as well as anal malformations are a serious problem for homosexual HIV-positive people as in this group the increased rate of HPV infection and the immunosuppression that gives the opportunity for the viral DNA to integrate into the DNA of the anal epithelium and cause cellular damage coexist.
What do anal warts look like?
Anal warts look like small moles which can appear in a variety of colours usually in the colour of the skin or in brown, white and pink shades. Their shape can be compared to that of papillomas and their size ranges from tiny just a few millimetres (undetectable) to 10 to 12 cm. In the case where the volume of anal warts has grown excessively, partial obstruction of the anal area is possible, creating significant problems for the patient which require immediate treatment.
Anal warts usually develop in clusters and may extend to other places adjacent to the anal area (vagina, urethra, penis, etc.). They often cause itching and burning sensation in the anal area and, in some cases, skin lesions can lead to bleeding.
What are the symptoms of anal warts?
Anal warts are found in and around the anal area. They start as small lumps that may be no bigger than the head of a pin. At first, they are too small to be noticed. They can develop a cauliflower-like appearance as they grow or when they gather together. Sometimes they can grow large enough to cover the entire surface of the anus and perianal skin.
Anal warts often appear without pain or discomfort. Other symptoms of anal warts are relatively rare, but may include itching, bleeding or discharge of fluid from the anus. A person with anal warts may also feel that they have a lump in their anal area, as well as a feeling of fullness of the anus and a feeling of incomplete emptying.
Warts can appear on other parts of your body at the same time you have anal warts. Genital warts in women can appear in the vulva, vagina or cervix. Genital warts in men can develop on the penis, scrotum, thighs or groin. Warts can also develop in the mouth or throat of a man with HPV infection. Oral sex with a person who has genital warts or deep kissing a person with warts on the neck can also lead to infection.
How are anal warts diagnosed?
The most appropriate doctor who can make a valid and responsible diagnosis of both intraproctal and periproctal warts is the qualified surgeon – proctologist. All people who present with anal warts should undergo the following diagnostic tests:
An overview of the perianal area. This examination is short and with this examination the specialist doctor-proctologist can easily diagnose the warts located in the perianal area, but also differentiate them from other diseases whose clinical picture has some similarities with that of warts, such as haemorrhoids, anal papillomas, ringworm, perianal fistula, transpurulent anal sweating, anal herpes, anal herpes, anal syphilis and perianal skin freckles. It is now preferred that the perianal survey is performed using a microscope so that even the most minute HPV lesions can be detected.
Rectal cytology test (Rectal Pap Test). This is a similar test to the Pap Test that women have to have to prevent cervical cancer. All people in whom perianal or intra-anal warts occur (men and women) should have an Anal Pap Test to prevent anal cancer. The Anal Pap Test is a simple, short (it takes about 2 minutes) and painless procedure that can be diagnosed in a few minutes.
Rectal cytology test (Rectal Pap Test). This is a similar test to the Pap Test that women take to prevent cervical cancer. All people in whom perianal or intra-anal warts (men and women) occur should have an anal Pap Test to prevent anal cancer. The Anal Pap Test is a simple, short (takes about 2 minutes) and painless procedure that can diagnose pre-cancerous lesions of the anus (malformations) in high-risk groups of people.
Anal fingerprinting. During the finger examination, the specialist proctologist looks for lesions that can be palpated in the anal area. It is very important to thoroughly check all quadrants of the anal canal. In addition, the tonicity of the sphincter mechanism is checked by finger examination, as is the prostate gland in men.
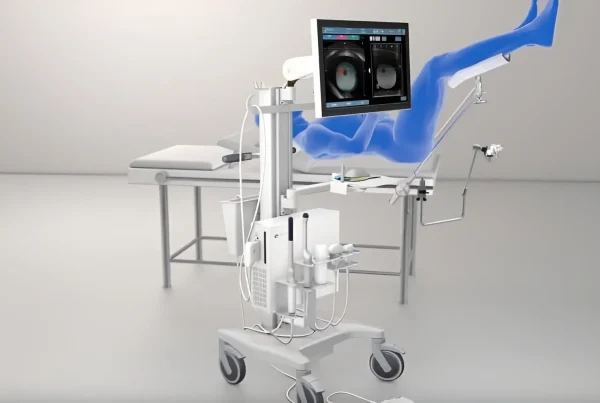
High Resolution Anoscopy (HRA). This test is very specialised and is performed by very few doctors around the world. It is used to find precancerous lesions and warts inside the anus. During the procedure, precancerous lesions are searched for using a special microscope.
Treatment for anal warts
Treatment of anal warts to be effective should include the treatment of both perianal and intra-anal warts, as well as the detection and treatment of precancerous malformations of the anus and perianal area. All of the above lesions have a common causative agent, the HPV virus, and therefore their treatment must be uniformly carried out by a qualified plastic surgeon. The treatment of lesions due to HPV infection (warts and malformations) should be performed by High Resolution Anoscopy (HRA). This is a procedure that requires training, expertise and experience. Proctologist Dr. Ioannis Dontas is one of the first physicians to apply it in Greece, after training in the United States of America.
In particular, treatment options include:
Local medication: These creams usually work best if the warts are very small and are only on the skin around the anus.
Topical medications that will freeze the warts (liquid nitrogen).
Topical medicines that will burn the warts (trichloroacetic acid, podophyllin).
Surgery: when the warts are either too large for the above treatments or are internal, surgery is considered. During surgery, the warts are surgically removed. The patient will be anaesthetised for the procedure. The type of anaesthetic depends on the number, size and exact location of the warts being removed. When there are many warts, the surgeon may perform the surgery in stages. An internal examination will also be done to identify and treat any lesions inside the anal canal.
Wart cauterization with surgical carbon dioxide laser (CO2 laser). A modern technique that offers a safe and effective treatment for warts. Through the use of the ultrapulse CO2 Laser in combination with a special microscope, even the most microscopic lesions are identified and eliminated and in this way the possibility of recurrence of warts is reduced to a minimum. This technique is one of the safest, most painless and bloodless techniques available and is the technique that can be used in the most common cases.
Anal warts and prevention
As mentioned above, anal warts are caused by HPV infection. Therefore, the vaccine against this virus if given in time significantly reduces the chances of developing warts. Vaccination is recommended for men and women up to 45 years of age and should ideally be carried out before the start of sexual intercourse, in order to immunise the body against the virus strains contained in the vaccine. The vaccine has been tested in thousands of patients and has been found to be safe and effective in preventing warts and anal cancer and other malignancies such as cervical cancer.
Other ways to prevent the transmission of HPV and anal warts include:
- abstaining from sexual intercourse
- using barrier methods such as condoms
- limiting the number of sexual partners
- stopping smoking
However, barrier methods do not fully protect against HPV as HPV can also be transmitted through direct physical contact, or even through contact with other objects